Type 1 Thursday – Bolus Gone Wrong?
Type 1 Thursday is BACK – and it’s all about the bolus!
Today, I’ll be answering a question from the audience about mealtime bolus gone wrong… How do you handle first high blood sugars, then low? Or high and steady after meals? Or low 3-4 hours after a meal? So confusing!
Do you have any experiences with mealtime bolus? How did you solve it? Let me know in the comments!
Also, do you have any questions for me to answer? I’d love to answer your question in a future Type 1 Thursday.
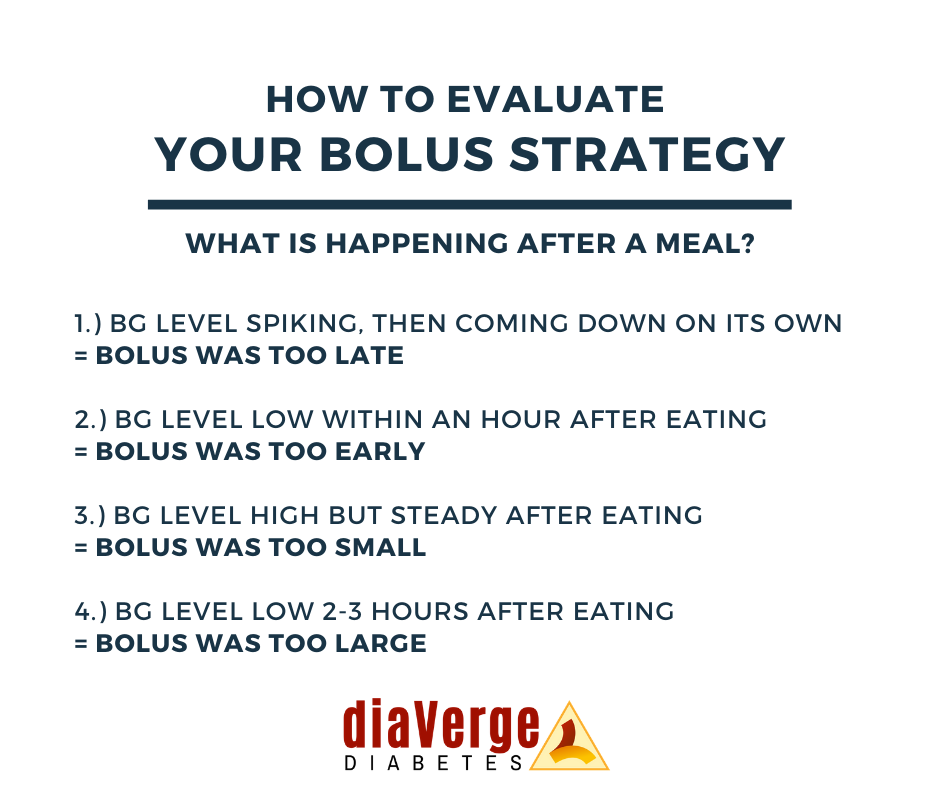
The bolus infographic from Diaverge.com that I mention in the video is this one:
Transcription
If you prefer a written version of the video above, here you go:
Type 1 Thursday – Bolus Gone Wrong?
I have a really interesting question today actually, because this is something that I’ve struggled with myself quite a lot. I got a question from the audience this time to answer.
“So, how do I time insulin for different meals? I’m struggling despite eating low carb, and I still spike sometimes dosing at the start of the meal and then go low one hour after. And if I dose at the end of the meal, I go high and then low three hours later? This is so confusing!”
Rachel
I do agree with Rachel, it is very, very confusing. It is difficult to figure this out. But I do have some rules of thumb that may help Rachel (may actually be a good reminder for myself, too) and maybe it will help one or two of you guys as well.
Dosing vs Timing?
As I see it, this can be both a dosing issue, but it can also be a timing issue.
This really comes down to first of all, what kind of mealtime insulin are you using? Are you using regular insulin as many people do on low carb? Are using some of the faster ones like Humalog or Novolog or Novorapid? Or are using the even faster ones like Alfrezza or Fiasp? It’s very difficult, as these insulins have different working time until they actually hit your system. Until you figure that out, it can be clue number one!
Clue number two is that it definitely can be a timing issue, but also a dosing issue. So let me go through this very, very carefully, point by point so that we don’t lose any details because that could be devastating!
– if you first spike blood sugar after your meal, and then you go low, that means that you took too much insulin. It was also too late, hence the spike first and then the drop. So, play around with that, maybe you need to dose a little bit less, or maybe you need to do the same dose but earlier.? So that can be one of the clues if that is your problem, which it was in the question.
– if you go low within the first hour, the amount of insulin you took was just too early because it hit your system before the food hit the system. So be careful and dose a little bit later.
– if your blood sugar goes high and remains high after food, your bolus or the amount of insulin that you took was just simply too small. You need more bolus for that particular food or that particular situation or that particular anything-that-you-know influences blood sugar (which we all know is about a gazillion things).
– Number four, which was also part of Rachel’s question, you go low two to three hours after food, that means that the bolus was too late. And definitely too much because your blood sugar dropped afterwards.
Those are the four different scenarios that I can figure out that may help. I shared this in a wonderful infographic from the beautiful ladies at diverge.com recently on my Facebook page, and it’s also above here in this post.
If you’re not recognising the patterns that you’re that you have. If you notice, for example, when you have certain foods, does the one or the other happen? If you have different timings of insulin, of course, this or the other happen? Or perhaps something completely new? Or, for example, if it’s the time of day – some people are more insulin resistant in the mornings than they are in the afternoons! So it can also be a timing issue, not just because of the insulin and when you took insulin and how much, but it can also be, depending on how or what time of day it is, because it just doesn’t always add up. It’s not always the same for people and especially not Type 1’s that are handling a lot of things at once.
I’m very, very happy to hear your experiences with mealtime bolus? Do you have any problems? How did you solve them? Have you maybe not solved them yet? Let me know in a comment below and I’ll be so happy to chat with you there.