What Strange Things Impact Your Blood Sugar?
What are the STRANGE things that make your blood sugar go either up or down, high or low? 🤔
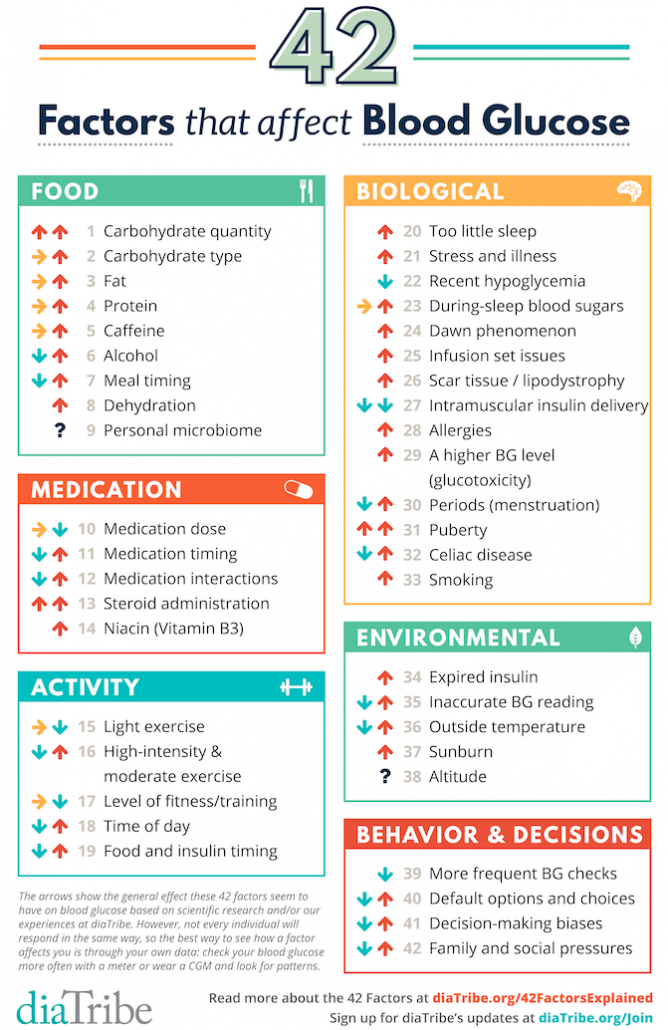
In this week’s Type 1 Thursday 💙 we discuss our personal experiences, based on Adam Brown’s graphic “42 Factors that Affect Blood Glucose”🩸
While some of these factors may be strange ones to impact blood sugars, I, of course, thought we should take it a step further. With diabetes being such an individual condition to live with, I wanted to know what the strange things are that impact YOUR blood sugar?
I asked this on my Instagram Stories, and got some amazing replies!
We’ll stick to the same categories as Adam uses in his graphic; food 🍽️, medication 💊, activity 🤸🏼, environmental 🌿, biological 🧬, and behavioral 😄, adding our own strangest things that impact blood sugars!
Strange Food Impacts
Let’s start with food because it is such a fantastic thing! I love food so much – I love eating food, enjoying food, everything. Because diabetes is such an individual thing to live with, I wanted to know what are the “strange” foods for you that has an unexpected impact on your blood sugar? Perhaps it probably shouldn’t have an impact, but definitely does?
Starting with your replies to my Stories, the first one is (of course!) porridge, or oatmeal. It really shoots people high in terms of blood sugar, and then someone said that they come down really low afterwards. Someone else said that “it’s not that healthy because it shoots you up to so high”. This is definitely a thing and I don’t think it’s unusual. Bread was another example, as well as pasta (starting to sense a theme here!) These are also blood sugar killers for myself, and dosing the correct amount of insulin for them is really hard (plus I’m quite gluten sensitive. The gluten free versions are almost worse because they have an even higher carb count because it’s made out of corn and and rice flour instead of the wheat.). Even the more complex carbs are not that easy. While many people seem to be able to eat it without problems, so it’s not always impossible! It just means that it’s a bit more challenging and you have to find the way that works out for you.
For me personally, a strange (although not so uncommon) thing to impact blood sugars is caffeine. I really do notice when I’ve had caffeine and not. Probably the strangest one I have in my repertoire is raw cabbage. If I eat raw cabbage, it will spike me, but if it’s either cooked or treated somehow, it won’t. This is a really interesting thing to me. I have no idea why. but I’m guessing it’s because of the vitamin C in the raw version impacting the sensor reading more than tactual blood sugar. But I’m not sure if that’s true at all. The opposite seems to work for boiled carrots being a bit of a challenge. But raw for some reason works for me. I just had two smaller raw carrots without any changes in blood sugar. difference.
Also, for me recently, maltitol, the sweetener that is supposed to have zero blood sugar impact, really does spike me quite horribly. Even if things say “sugar free”, “low carb” and even “keto”, it’s not a free grab-and-go, no, no, no! I still have to look at the label and not take it for granted.
However, when I was young, we had a science experiment in school where we grew some sprouts (alfalfa?). I remember eating those and my blood sugar would actually drop. I wonder if anyone else has noticed that? I’m guessing it’s somehow related to, intestinal flora or gut flora or something like that? (If anyone else knows what’s going on there, please do share!)
Medications…
The only one I can I can really say is that some antihistamines cause a raise in blood sugars. And, of course, certain interactions, like for example, steroids make you more insulin resistant, which is not really that strange, but can be unexpected.
If you have any medications that unexpectedly raises or lowers their blood sugar do share!
Strange Activity Impacts
This one is a bit funny. Every time I vacuum my blood sugar plummets (and I know I’m not alone in this but I don’t see mentioned much)! I don’t understand what it is about it? Maybe it’s just my really vigorous, pissed off version of vacuuming that makes my blood sugar low? I always have to ask my husband to do it and I trade for something else, just so I won’t go low.
Environmental Factors
Someone commented about how cold weather makes their blood sugar go low. For me, it’s almost the opposite. Cold weather makes my blood sugar go high, whereas a warmer weather lowers it. I’m guessing for this person that sent in that comment, it’s the other way around? That’s really interesting, because sometimes you just really feel like the weather impacts your blood sugar. And you know what it really does! This is strange to me, because technically it shouldn’t. Anyway, this can, of course, be during sleep, too. If it gets too warm in the room while you sleep, or too cold your blood sugar also react according to your personal weather blood sugar reaction profile.
Strange Biological Factors
The biggest one here, of course, is stress and anxiety. I always say, and I feel like a broken record here, that it is blood sugar killer number one. It can really make or break your blood sugar levels. That’s why stress management and stress relief is so important in diabetes care for me. Stress and anxiety raise my blood sugar, no matter whether it’s a hard meeting with with a boss or for a project, or even something fun like holding a workshop or public speaking engagements, stuff like that. Or you know, it can be just family, which can be a source of stress and anxiety! Another comment is that “anxiety comes in when my blood sugar is low”. Hypo anxiety is absolutely 100% real. Dreams can really impact your blood sugar, if you have a scary dream, you can get really stressed and scared.
Something personally stress-inducing for me right now is dealing with my health insurance. They’re being the acronym of PITA, which is highly applicable to them right now! Dealing with health insurance, or diabetes admin in any way or form is a form of stress and anxiety.
“For me everything raises my blood sugar” Yeah, that’s actually very true. But also quite biological. As we only have one thing to lower our blood sugar, which is insulin, and there are four or five other hormones in our bodies that raise it. Meaning that insulin is fighting a hard fight on its own! This gets especially challenging if you then don’t, in addition, produce the insulin and have to be a pancreatic understudy. So it’s really not easy.
Someone sent in this fantastic comment in my Stories, that petting animals, because it reduces stress, really increases their insulin sensitivity. I love this because I love the reason so much!
Hormones…
It’s really interesting, and I’m only bringing it up, not because it’s that strange, because, you know, it’s biological (and logical?), BUT because there’s so many people who don’t maybe have it in the back of their minds. Periods, PMS/T – times of the month – but also time of life (puberty, pregnancy, menopause…) can also really impact blood sugars. See it as a small reminder to track your cycle quite closely. That way, you can be more proactive rather than reactive in caring for your blood sugars.
Another biological reason for strange blood sugar impact is jetlag. Your blood sugar can go up or down depending on timezones and traveling across them. And it really doesn’t seem logical at times! Unrelated (but perhaps not after all?), have you ever noticed that your vitamin D levels can impact your blood sugars, as well? If your vitamin D is too low, you can be more insulin resistant, for example. When it is in a normal range, or in a good range, then you are more sensitive (I know this has been a topic on Instagram a while ago!).
Strange Behaviour
There are a lot of things that you can do behaviorally, that may or may not help you in caring for your blood sugars! My biggest example here is being out of your normal routine and how that impacts your blood sugars. It can make it more difficult and more challenging to keep blood sugars that you are used to as normal. That can also be of course due to jetlag, or something like that, of course. But also, if you need to do something different, I’ve had two very early mornings here in the past couple of weeks, where I had to get somewhere else for a meeting, and that definitely changes my blood sugar management for that day, only because I’m out of my routine and comfort zone.
I’m loving all these fantastically weird and wonderful things that impact blood sugar levels for you guys, and for myself, as well. I hope you’ve learned something!
What did we miss?! Leave a comment and let’s chat more. 💬
Disclaimer
The only purpose of this video and website is to educate and to inform. It is no substitute for professional care by a doctor or other qualified medical professional. This video and website is provided on the understanding that it does not constitute medical or other professional advice or services. Instead, we encourage you to discuss your options with a health care provider who specializes in treating Type 1 Diabetes.
blood sugar, impact, strange, insulin, diabetes, anxiety, stress, blood sugar levels, biological, jetlag, high, routine


