Blog
Gratitude
Reflecting on all the things we have to feel gratitude for is sometimes overwhelming, even if they’re all little individual sparks of joy in our lives.
Sitting here, being so overwhelmingly grateful that I have the chance to start yet another year. A year that I can choose to shape and form in exactly the way that I want to. A year where I’m more determined than ever to inspire those around me to become healthier, happier and feel more joy (not unlike my own goals!)
Throughout my life with T1D as my constant companion, starting a new year of life hasn’t always been a given. Yet, for many years I took it completely for granted. No more.
I found this great quote, which I think is very fitting today:
“I know as a woman I’m supposed to be afraid of getting older but I love this shit so much. Every year I sink deeper into this bath of unapologetic realness and it’s amazing.”
Bunmi Laditan
No matter how bad the world may look today, there’s always, always, always something to be grateful for. So much gratitude in the world!
What are you grateful for today? 🌟
(Post originally posted on my Instagram account – @hannadiabetesexpert
Type 1 Thursday – Stress & Blood Sugar?
What does STRESS have to do with your diabetes management?
Have you noticed that your blood sugar reacts in an unexpected way, either up or down, when you’re stressed? We can distinguish between physical and emotional stress, and, sadly, we are way more emotionally/mentally stressed today than ever.
Today, I talk about why this happens and what causes it, along with stress prevention and coping mechanisms. You can read a written version below if you can’t watch the video.
Have you noticed that stress impacts your blood sugars? How? Leave a comment!
Transcription
Stress and the impact the stress has on your blood sugar management is sometimes overwhelming, because it can make things a little bit more interesting than intended to be.
Here, I’m going to cover what happens in your body when it experiences stress, and how we can alleviate it and what we can do to cope with the stress that we do face, perhaps even on a daily basis.
What happens to blood sugar, or rather, why does it happen that blood sugar gets impacted by stress? It is our beautiful stress hormones like cortisol, adrenaline, noradrenaline and epinephrine, that are impacting your blood sugar. They tell the liver that your body needs more energy to cope with this stress. That’s why your blood sugar will react either way, in the vast majority of cases, your blood sugar will rise when you are under stress. But there are also instances, which I’ve experienced myself where, during stress, your blood sugar unexpectedly does drop, which is unexpected, and you have to roll with the punches. An example of this, that maybe most people with diabetes can relate to, is Dawn Phenomenon. This is when our stress hormones tell our liver that “hey, it’s time to wake up. Let’s get some sugar in the blood from your storage system and get this party going.”
There are two main forms of stress. One is physical stress, for example, if you had an injury, or if you exercising super hard, or you’ve gone through surgery or some sort of physical trauma, and infection, then definitely your body is under stress. That’s also why we can see when we are getting sick or that when we are sick, that the blood sugar’s can rise, because it is a stress for the body, and stress hormones are released and the little sugar party is going on in your body.
It can of course also, and it may be more usual for us in today’s society, that it’s emotional stress. This can be things like, being overwhelmed or you’re just too busy, you have too much to do, too much on your plate, anxiety, your phone going off all the time, the train is late… Essentially, it’s what becomes more of a psychological stress. But that can also have an impact on your blood sugar, which is why I bring it up. The fact that we experience so many things as stressful has been left throughout our evolution. When we had to be afraid of wild animals in nature, so that we had that quick release of energy, so that we could run far, far away from that mountain lion/bear, and get into safety. That’s why our body reacts with the sugar rush when we get stressed. The problem is today though, that some things that shouldn’t be stressful are interpreted by our bodies as stressful. It can be nutrition, for example, too much sugar can be a stress for the body. It can be, as I said, the train is late, or your phone’s going off every second. There’s so many things that stresses us today that didn’t use to stress us. This also means that we can see more volatility on our blood sugars because of that.
What can you do to mitigate stress? Find patterns. Is there certain situation every time that you do it, that causes you to stress and have a blood sugar spike, for example? Is there something that you do in your daily life that you don’t feel well doing? Is there something that goes against even your own values? Could that be stressing you? Find a pattern, so that you know how to react! When you have the prediction, you can also prevent it. It’s really important to pay attention to this (and with everything else) to see the patterns in it, so that you can just simply prevent it. Bear in mind that this is very individual. What stresses me for, example, may not stress you, you lucky person! And what stresses you, may not stress me at all. It’s very individual and we have to see on an individual level how we are impacted by stress.
What are some coping mechanisms for stress? Cut down on the nicotine, alcohol and caffeine, all of the stimulants that we may use under the impression of that it will help us with stress. It will probably stress our bodies even more. Recognising that we are tired and doing something about it, taking a break. Physical movement also really helps stress. Make relaxation a priority, if you don’t make space for it, it won’t happen. You know that with a lot of other things in your life perhaps, but making space for it and making time for it does matter. So make sure you schedule in relaxation. Make sure you also have a sound sleeping schedule, so that you make sure that you sleep enough during the night.
Accept things that you cannot change. This is really hard, but it’s really worth it. It does remove a lot of stress. Improve your time management, maybe that’s where you’re lacking a few tools? And my personal favourite jump on the No-train. Say no to things that do not light you up, that you are not excited about and that you know that you won’t be enjoying.
When we are in the stress situation, how can we alleviate it? This goes hand in hand with the coping mechanisms mentioned above, but how can we alleviate it as well as we can? Movement. do move daily. How about actually scheduling a holiday? That could be something great right? Listening to your favourite music for example, that could be an amazing stress reliever. Take up a hobby that takes your mind away from the from the stress. How about meditating? Meditation can really calm you down, along with breathing exercises. Breathing deeply can really distress you quickly! Or how about taking up yoga, stretching your body and feeling and really being in tune with your body also helps stress.
Relaxation cannot coexist with stress
Do remember that relaxation cannot coexist with stress. If you’re relaxed, you cannot be stressed at the same time.
I would love to hear if you’ve noticed that your blood sugar has been impacted by stress? What happened? How can you change it until next time? I can’t wait to chat with you further in the comments below.
Ps. Are you looking for a stressless retreat to soak up the last of the summer sun, learn from international health experts, spend time with likeminded people, all in a place too gorgeous to miss? Join me at the amazing The Low Carb Universe 2019 in Mallorca, Spain in November!
All about my latest HbA1c…
“Your A1c is 4.8%”, she said with disbelief in her voice.
“No way”, I replied, laughing, “it must be an error!”
“It’s time for your yearly blood work anyway, let’s throw in an HbA1c, too. The labs margin of error is a lot less”, she mentioned.
Excellent suggestion!
Well, the lab results came back at 4.7% (29 mmol/mol)! My lowest ever reading, by far. And that without significant lows – Dexcom shows 6% lows for the past 90 days (a few of them are pressure lows too.)
I remember just a few years ago when I could easily have added a 1 in front of that result and it would’ve been my reality. I remember the pain, frustration and hopelessness I felt. I am reminded of my war wounds from having battled T1D for 34 years.
And I finally feel a sense of freedom. Freedom of having found things that work for me and my diabetes management. Freedom in the feeling that normal, healthy and healing blood sugars ARE possible, even after living this long with this disease.
This by no means means that I never have problems. That I never have days when it’s all shit. Or never have moments I want to give up. But there are less of them now.
If I can do it, so can you! 🙌🏼 Share your achievements with gratitude – they are worth it to be acknowledged!
Thank you for your support and for following me on my diabetes journey. 🙏🏼 You are the best.
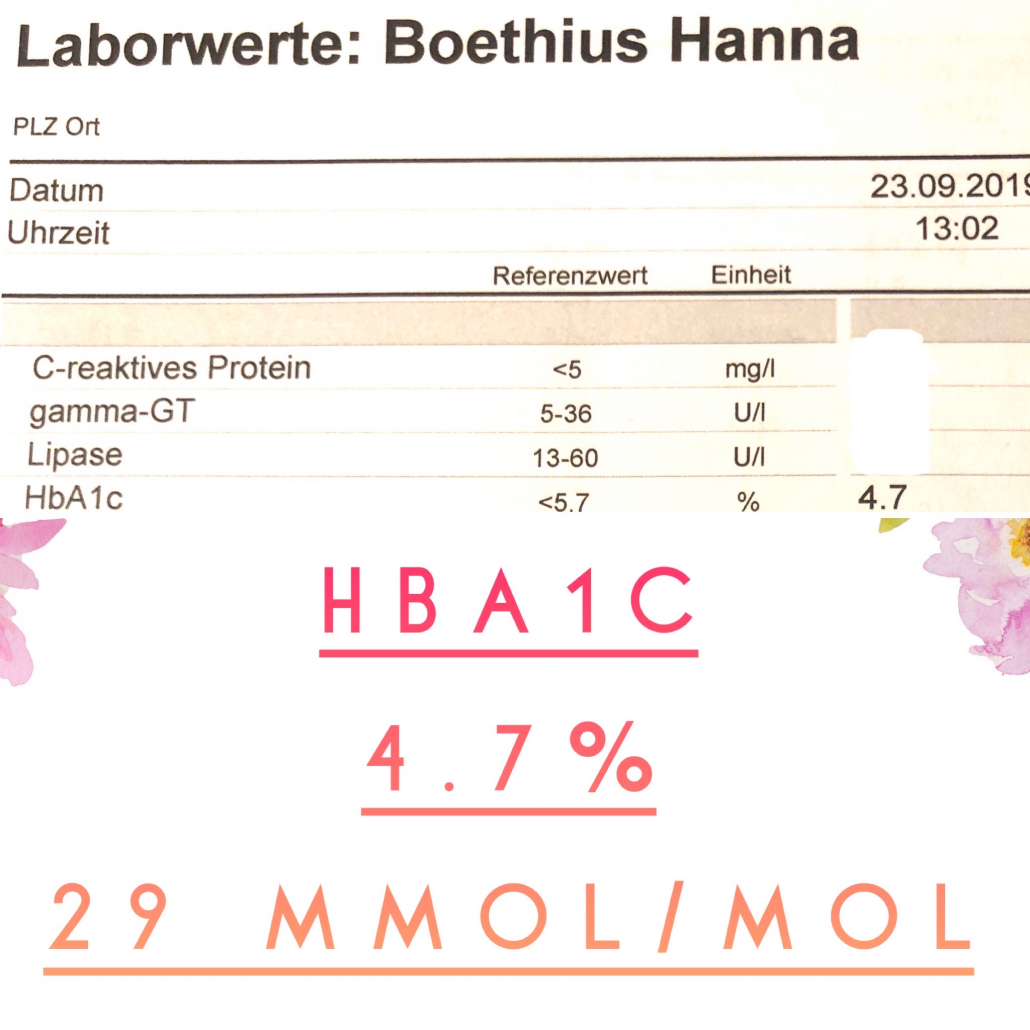
Ps, do you want to know my HbA1c lowering formula? Watch my Type 1 Thursday episode about it here!
Type 1 Thursday – Hydration, why so important?
How important is hydration for diabetes? What can it cause if you’re not hydrated?
I’ve noticed it myself. Sometimes, if I have a particularly stubborn high (or event borderline high) blood sugar that won’t come down with my usual line of care, it may very well be that I’m a bit dehydrated.
But is that the whole story? In this weeks episode of Type 1 Thursday, I go over the main factors why hydration is important, what signs of dehydration is, the causes, and how all this can impact your blood sugar management.
Do you consider hydration an important part of your diabetes management? Why, or why not? Let me know in the comments!
Transcription
If you prefer to read about hydration instead of watching the video, here is a transcribed text version for you:
We all do it every day, hopefully. And we may not be paying enough attention to it though, which is why I wanted to make a point of it today: hydration, and how important hydration is to a diabetic or person with diabetes, depending on which you prefer.
What causes dehydration, and what can it cause if you’re dehydrated? Dehydration is a higher risk for people with diabetes, because of high blood blood sugars being dehydrating for the body. Even if you don’t have super high blood sugars, or maybe you are someone who is up in the 70 to 90% it time in range of blood sugar. But even then we do have those few circumstances when the blood sugar does go up so that we have to pay attention to our hydration.
High blood sugars don’t just cause dehydration, dehydration can also cause high blood sugars. I know this for myself, for example, if I have a more stubborn, higher blood sugar than I would like insulin is not really taking as it should, movement doesn’t help, insulin neither, all my normal strategies of trying to get my blood sugar down. Sometimes, it can actually be that you are a bit dehydrated! In that case, that’s why your blood sugar has gone up as well, because the body doesn’t have enough liquid to actually keep that blood sugar moving in the body. One doesn’t necessarily cause the other, they can both cause each other. It can be a vicious loop, unless you pay attention to it.
What are the symptoms of being dehydrated? The obvious thing is thirst. If you’re thirsty, you’re probably quite dehydrated and you should fuel up with some water. You can have a headache, often a creeping on headache can also be a sign of dehydration. Dry eyes and dry mouth, I know for myself when I have a higher than normal blood sugar, I can definitely feel my eyes being like a little bit sandy, and my mouth feels like it’s been swiped with about 15 cotton balls! You can become dizzy, especially in hot weather, for example if you’re dehydrated. You can become tired and sluggish. And, if you when you go to the bathroom and your urine is dark, that can also be a sign of dehydration.
What causes dehydration? One I already mentioned was high blood sugars. But as you remember, high blood sugars can cause dehydration, but the dehydration can also cause high blood sugars. Yhe jury’s still out on which one is which! Other things are you simply drink too little water, that is very likely one of the causes. Hot weather or strenuous exercise, so if you’re sweating more than normal, can be a contributing factor. It can be alcohol, for example, that dehydrates your body. Diarrhoea or that you’ve been vomiting can also dehydrate your body.
Why does dehydration happen? And why in relation to high blood sugars? When our blood sugars are high, the kidneys try to filter as well as much of it out as possible. This means that you actually filter a little bit more of blood through your kidneys at that point, which also brings with it water. In a simplified explanation, that’s why we get dehydrated and can feel dehydrated when our blood sugars are higher. Actually, the main point in diabetic ketoacidosis is not necessarily the ketones, for example. Ketones are not bad in limited amounts. It’s also not necessarily the high blood sugar, but it is the dehydration. The really dangerous part of a DKA, and especially if it has come to vomiting and other symptoms of DKA can bring with it, it is the dehydration that makes it dangerous. Please watch out so that you don’t become too dehydrated, as it can also be a contributing factor to the diabetic ketoacidosis. And, I can’t forget, every time I talk about DKA, I cannot miss the fact that it can only be caused by a lack of insulin in the body! This can be a relative lack of insulin in the body, when the body is simply not getting the insulin that it needs and requires to work properly. That is why DKAs happen – it’s not necessarily just because of the high blood sugar – the root cause is always too little insulin. Diabetic ketosis is not the same as ketosis, they are two completely different things. You can see and read my further thoughts on DKA av ketosis here!
Anyway, back to the topic! Dehydration can also cause a lack of electrolytes. If you’re severely dehydrated, you should and may have to go to the hospital to get IV fluids with electrolytes.
How much to drink is another question I often get and that is a little bit of a tricky one, because it is very individual. It entirely depends on how active you are, on what you do and depends on what shape your body’s in. It depends on so many factors! As a rule of thumb, I personally try to drink about two litres of water a day. This also helps me flush out any things that aren’t supposed to be there and also help to stabilise my blood sugar.
Thank you so much for watching. I can’t wait to chat with you more in the comments! If you have any questions, comments or experiences that you want to share with me, please leave them in a comment below, and I’ll happily chat further on over there.
Just remember kids and sweet friends, drink your water and keep hydrated!
Type 1 Thursday – Why Real Food?
Real food is actual food, food that comes from nature and is not refined, made in a factory or tampered with by humans. And no matter of what way you choose to eat, be it keto, paleo, vegan or otherwise, we can all agree that real food is what is the best for our bodies, health and blood sugars.
But why is eating real food so important? And especially so if you live with diabetes? In this week’s episode, I outline a few quick points. Watch the video, or read the transcription below, and let me know your thoughts!
Ps. If you do like the concept of eating real foods, why don’t you join me and an amazing group of people at The Low Carb Universe 2019 in Mallorca, Spain in November? Incredible international health experts, amazing views, movement, joy AND 100% real food! You can book your ticket here!
Do you eat mostly real foods?
Transcription
If you prefer to read to learn, below is a text version of the video about real food above. You can also read why low carb is a great option for Type 1 Diabetics here!
Why Real Food?
Today I have quite an exciting topic, if you ask me, because my background is within nutrition. My topic for you today is the importance of eating real food.
I am so happy to hear your comments and ideas and thoughts about this topic or any other topic, actually, I’m easy that way! Jot them down in a comment below and I will be happy to chat with you there anyway, about real food.
If you ask me, that is the only topic where we can actually agree on, no matter what kind of diet we choose to follow or eat. I don’t really like the word diet, but I choose to use it anyway, as it’s normally the one used. The thing is, whether you are keto, paleo or vegan, or, well, maybe not the Standard Western Diet, actually, because the importance of real food may not be so, so big there. In any other diet that you may or may not be following, I think real food is the one thing that we can agree upon, that it is very good for us.
What I define as real foods is foods that don’t have a label. Real foods actually comes from nature, which is quite rare, if you think about the standard Western diet. It is foods like meat, poultry, eggs, fish, seafood, vegetables, and all these things that actually come from nature and from the earth and not through a factory, or from a factory or has been tampered with too much with by human beings. They’re just as clean and natural and real as possible. That’s my definition of real food, so that we’re all on the same page throughout this discussion.
The main point of this is that real food has no additives. What additives often do, is that they mess with your blood sugar. For example, maltitol is a classic example of this! It is a sugar substitute that still affects your blood sugar. Don’t be fooled and eat that, although it’s supposed to be great and “diabetic friendly”, can be labelled whatever you want to be labelled with whatever health claim. They still include things that are really not good for your blood sugar and really not good for your health. In effect, you’re not doing yourself any favours by buying these “health foods”. No additives, so that they can’t mess with your blood sugar, in this case, if you are diabetic, or live with a blood sugar problem.
If you are going to venture into that kind of a sphere with pre-made foods, I have as a rule of thumb for you. The food item can include five ingredients, and those five ingredients all have to be recognisable to me, I need to know what they are, without googling, because that’s cheating. Then, if I approve all of those ingredients, then yes, absolutely, I will buy it and consume it and enjoy it. But if that is not the case, it will most likely go back on the shelf! “I see it, I love it, I want it, I checked the carb count, put it back”, is pretty much like going to the grocery store with me. My poor husband, I mean, seriously… Anyway, 5 ingredients that are recognisable otherwise, to me, it is not worth the gamble of a possible really high blood sugar or a possible low blood sugar, because I’ve overdosed insulin. It’s just not worth the hassle for me.
What are the top my top three “watch out” ingredients for additives in food?
If you do live in the States, or a similar kind of an environment, high fructose corn syrup. Just stay away, that can really mess up so many metabolic markers within you, so much of your metabolic health can be ruined, because of the consumption of high fructose corn syrup. It’s just so highly refined and so highly tampered with that it’s not really worth it to consume in my opinion. It’s no longer food, it is just factory made.
Number two, trans fats, man made oils, trans fats, are really not good for you. They add a lot of unnecessary strain on your body and your metabolism (that you can just actually fix with eating real food). Adding real fat such as butter, avocado, olive oil, things that are actually not man made, but is made by nature, is a lot better for you than highly refined and processed fats.
Number three, and this can be a tricky one, I do admit it. So bear with me before you slam down the lid of your laptop or turn off your phone, but it’s artificial sweeteners. And with that I really mean the artificial sweeteners, the ones that have been made in a factory. Maybe stevia is fine for you, if you enjoy the the flavour of it. And monkfruit can also be fine. Erythritol to a certain extent, absolutely. But things like aspartame and things that we don’t really know what it’s doing with our bodies yet. It’s definitely not natural in any way or form, and that I would be careful with. I remember growing up, this was a huge thing, as long as there were artificial sweeteners, then, hey, this product is a go! I was raised in the 80s and 90s, when it was still a little bit more controlled what people with diabetes should be eating. I had to eat a lot of terribly sweetened things. It’s been shown in studies since that for example, fructose, which we thought back then was the holy grail for diabetics, can actually clog up your liver, so that it can’t do its job properly. Then your whole metabolism might be damaged.
There’s a lot to be said about this stuff, of course! These three things impact your gut health, they can have an impact on anxiety levels, they can, as I said, clog up your liver, so that can do its job properly. And other things like your skin and other things that are really important for us to work properly. These additives can make an impact on our health, and that’s not very good, is it?
I do want to sort of give a special warning, I did touch upon it a little bit at the beginning of this. For example, “keto foods” some of them or “vegan food” or whatever it’s labelled, heart healthy, don’t even touch this stuff is not healthy for you at all. Don’t trust the labelling on the box! Look at the ingredients, does it have five ingredients? Do you recognise them? Buy it, if you think you’re going to enjoy it, if it doesn’t, maybe you should rather leave it alone? “Foods”, such as salad sauces, sauces, spice mixes, soups, ready made things that you don’t think will have an impact can actually contain a bucket load of sugar and will impact your blood sugar. Stay with the real food is my opinion! It’s better for us, it’s healthier for us, and we’re going to feel a lot better.
If you’re just starting out from, for example, a standard Western diet, to going to more into the real food way of eating, then I really suggest you adopt the 80/20 rule, so that 80% of the time, on work days, you eat real food, and on the weekends, you can still have a bit of what you still think is fun.
I would love to hear from you. Do you eat mostly real foods? Let’s talk in the comments below and I can’t wait to see you next time.