Travel Checklist for Diabetes
Maybe you’re planning a trip soon and would love a travel checklist for diabetes?
(I made you a travel checklist for diabetes below, make sure to check it out!)
What is necessary to bring along on a long trip with diabetes?
Sometimes I feel like diabetes just has it’s own luggage to bring along, physically as well as emotionally.
The emotional luggage we’ll have to discuss another time, because this time I want to talk about the physical luggage Diabetes brings along. Especially when traveling.
As if packing for a trip isn’t stressful enough (“what shoes should I bring?”, “does this dress go with that jacket?”, “what make up should I bring?” and “WILL IT ALL FIT IN MY BAG?!” – you get the point…), as an added bonus, you also have to haul around on all the stuff that you need for diabetes to keep in line.
I always bring all my supplies in my carry on bag when I fly. That way it’s harder to lose it, and the insulin stays at the right temperature throughout my trip.
The size of said carry-on bag has changed, though, in favour of trying to save my shoulder from falling off from carrying all the heavy stuff. Now I bring along a small, cabin sized wheelie bag where I have all my supplies, from insulin, to pumps, to test strips, to hypo treatment.
I also deposit a few things in my traveling buddy’s, usually my husband’s, bag. At least that way, if I lose my carry on, I’m not completely stranded in terms of diabetes. He has an extra blood sugar meter and test strips, and insulin with emergency-syringes. And glucose tabs. One can never have enough of those.
While I make sure to bring along most things on my travel checklist for diabetes, I don’t always bring everything.
Like ketone sticks, for example. I don’t usually bring those, unless I’m traveling somewhere really remote with no pharmacy within the next hour or so of driving. I figure that I can buy them pretty much anywhere I go.
On the other hand, insulin and BG test strips can get really darn expensive, not to mention inaccessible without a prescription, unless you prepare properly and take enough with you for your whole trip. “Enough” here means way too much, by the way. You never know what might happen, so it’s better to be prepared for most things that may happen.
Food
And, pretty please, get organized and bring your own snacks. Food on the road is generally beyond terrible, and like that you know you can at least eat something. I bring things like nuts and dried meat and other cutleryless foods on the plane, whilst in a car or on the train you can get a little more creative. This time around I’m going to make low carb pancakes and wrap them up in foil to bring along on my long flight, as I know from experience that food on flights is never good.
Another note regarding food, please don’t get fooled by the “need” to snack, which is most commonly masking the fact that you’re bored out of your brain.
Water
Traveling by plane is like sitting in the middle of the desert, although maybe not quite as warm. It’s dehydrating like nobody’s business! Being hydrated can really be one of the keys to better diabetes management, so please do us both a favor and DRINK A LOT OF WATER! (and skip the booze up in the air, but that one is evident, right?)
Security
Getting through airport security can be a lot easier than it’s made up to be. This is of course assuming that you don’t meet an a-hole security agent.
In my 30 years of living with diabetes, having traveled to many different parts of the world (although I have MUCH left to see and visit!), I’ve been stopped exactly twice at security. Once for my test stripes (what, you didn’t mind the syringe full of potentially very deadly stuff in my bag? Ok, then.) And once because my pump set the alarm off. In both cases it was easy to explain, and I didn’t even have to show my medical certificate. Security agents see so many diabetes supplies on a daily basis; they’re barely phased by them anymore. At least within Europe.
Now, I’ve heard that US TSA agents can be a little trickier to handle. For example, they have no problem jeopardizing your super expensive medical equipment and tell you to go through the full body scanner wearing your insulin pump, for example. I would insist on the pat down, not risking any breakages or malfunctions. This of course means that it might take a little longer for you to get through, but it’s worth it, and as long as you know about it, you can plan for it.
The bottom line is, as long as you’re nice and cooperative (enough) to them, they’ll usually treat you with the same respect.
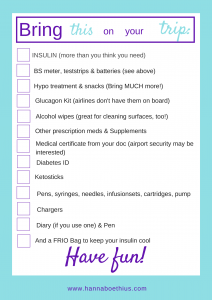
Anyway, let’s check out the goodie in this blog post, my Travel Checklist for Diabetes.
These are the absolute essentials that you need to bring with you (or at least ocnsider bringing with you). If you think “I’ve never needed that before”, you should probably take it along anyway, as traveling can make your body do some funky stuff.
Travel checklist
- Enough insulin to cover the days you’re gone (this should be a no brainer!) Make sure you bring both basal and bolus insulin, even if you’re using an insulin pump. You just never know…
- Blood glucose meter & enough test strips, extra batteries (it might even be good to bring an extra BG meter.)
- CGM sensors
- Keto sticks (As I said, I don’t always bring them)
- Glucose tabs (or whatever you use to treat a hypo) (Bring too much of this, you never know what your body think of your new location.)
- Snacks. (See above)
- Glucagon Kit (most airlines don’t have these on board their planes. Better be safe than sorry!)
- Alcohol wipes (these are great, not just for setting infusion sets and cleaning fingers, but also for wiping surfaces like tables, handles or cutlery that seems unclean.)
- Other prescription medication and supplements you may be taking (easy one to forget, trust me. I’ve done it before.)
- If you’re going somewhere really warm (lucky you!), bring something like the FRIO bag to keep your insulin in. (http://www.frioinsulincoolingcase.com)
- Medical Certificate (This can save you at security checks!)
- Diabetes ID (If you’re found unconscious somewhere, I’m sure you’d prefer that the EMTs knows what you’ve got.)
- If you’re going somewhere remote, bring a glucagon set. (Again, you never know.)
- Your BG diary, if you use one. (Otherwise there’s some great apps for that, for example www.glucosebuddy.com or www.mysugr.com)
- Address and telephone number of your doctor’s office.
If you are on injections, also bring:
- Insulin pens, plus back ups
- Pen needles
If you’re on a pump, also bring:
- Your pump, as well as possibly getting a back-up pump. (This can be ordered from your pump manufacturer.)
- Batteries/Power adapter
- Cartridges (if your pump uses those)
- Infusion sets, or just enough of patch pumps
- Syringes/pen for emergencies
- Basal insulin for emergencies
If you’re planning a pumpcation (vacation without your pump):
- Your action plan, that you’ve talked to your med-team about
- Pens and needles
- Basal and bolus insulin
It’s better to take too much than too little!
I’ve made a pretty print out of this list that you can print out and tick off the boxes as you put the items into your bag.
Click here to download the list: travel checklist diabetes
What are your best traveling tips? What can’t you travel without? Let me know in the comments!